ENJOY FREE SHIPPING ON ORDERS OVER $99
ENJOY FREE SHIPPING ON ORDERS OVER $99
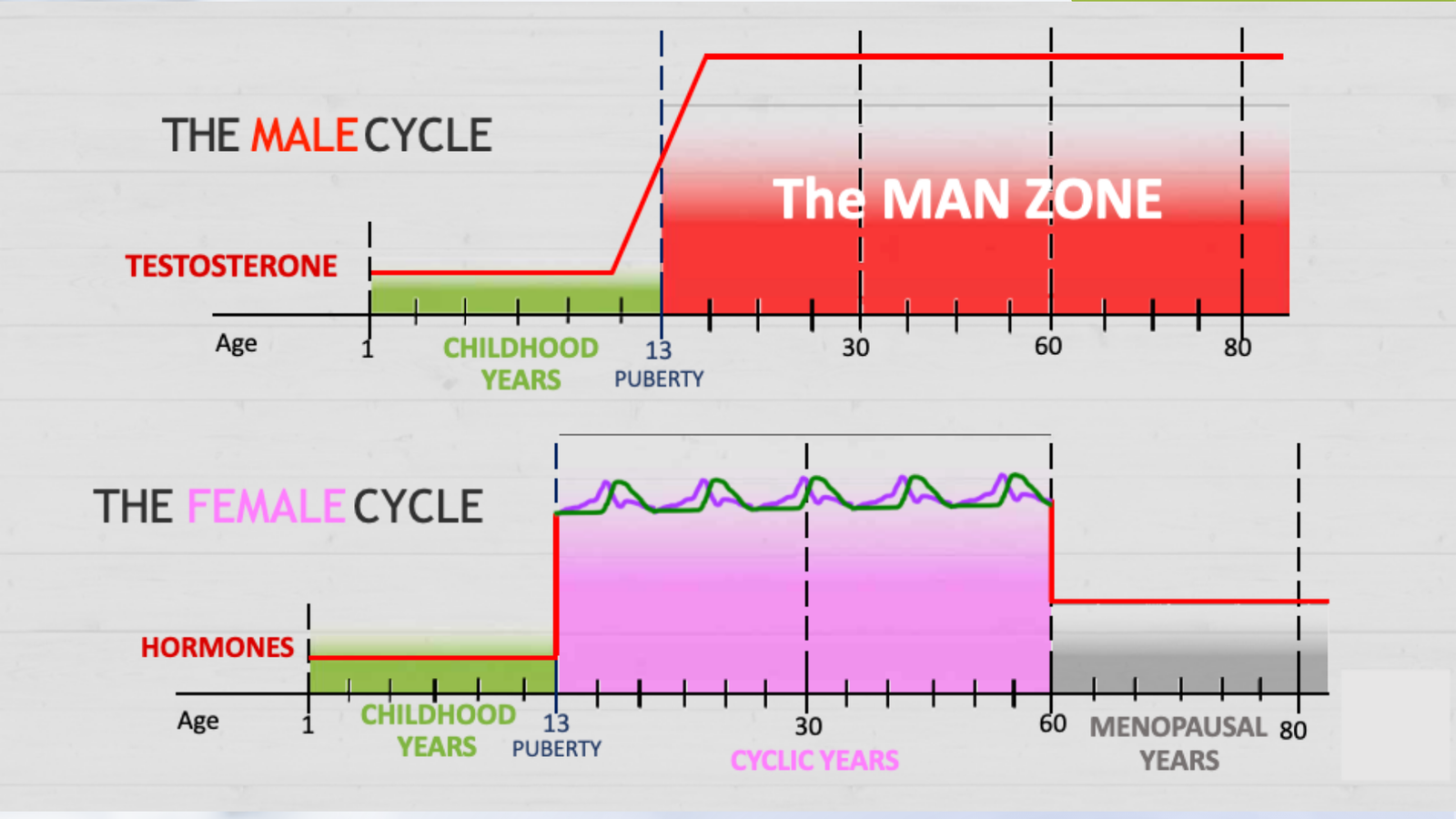
Menopause, Andropause, and the Art of Hormone Restoration
November 03, 2025 2 min read
The “Universal Syndrome” That Isn’t
In many industrialized countries, menopause is framed as a guaranteed storm: hot flashes, night sweats, mood swings, weight gain, and brain fog. Yet numerous traditional populations report a quieter transition. The difference isn’t a pharmaceutical gap; it’s a lifestyle gap—better mineral status, lower toxic burden, stronger circadian rhythm, more daily movement, and stronger social bonds.
This reframing matters. When women assume the storm is inevitable, they brace for it instead of building resilience in advance. When they focus on restoring safety signals to the hypothalamus, supporting gut–liver pathways, and strengthening metabolic health, the transition frequently becomes steadier and kinder.
Men and Midlife: Andropause Without Alarm
Andropause can look like fatigue, irritability, lower libido, and a thicker waistline. Lab numbers may slide, but the why matters more than the what. Chronic stress, visceral fat, poor sleep, and blood sugar swings suppress testosterone production and conversion. The good news: men who rebuild sleep, lift heavy (safely), walk daily, get morning light, and replete minerals often see both symptoms and labs improve.
The temptation to “fix the number” with pellets or injections is strong. Yet those therapies can trip negative feedback loops that reduce natural production, making long-term independence harder. Restoration strategies not only lift energy and mood; they keep options open.
Replacement vs. Restoration: Choose Your Path Wisely
Hormone Replacement Therapy (HRT) and Testosterone Replacement Therapy (TRT) can offer short-term relief for select patients, but they’re not neutral. Potential side effects include blood thickening, sleep disturbances, prostate stress, and clot risks. More fundamentally, exogenous hormones can signal the brain to downshift its own production.
Restoration focuses on inputs: nervous system balance, mineral sufficiency, gut-liver integrity, protein-forward meals, and strength training. When the inputs change, hormones often recalibrate. Bioidentical options may serve as a bridge under clinical supervision, but the destination remains the same—self-regulation.
A Practical Framework: Restore in 21 Days
Start with three non-negotiables and expand:
-
Morning: sunlight exposure, mineralized water, protein + greens breakfast.
-
Midday: walk after meals; posture resets; cruciferous veggies and color.
-
Evening: digital sunset; journaling; consistent sleep schedule in a cool, dark room.
-
Daily: strength training 2–4x/week, walking every day, fermented foods, joyful connection.
-
Optional: targeted botanicals/adaptogens and digestive bitters as personalized support.
Measure progress by lived experience—energy upon waking, steadiness of mood, digestion, sleep quality, and recovery. Labs can confirm the trend.
Rethinking Birth Control for Teens
Putting young women on hormonal contraceptives as a default “solution” for cycle issues can disrupt nutrient status (notably B6 for serotonin balance), skew clot risk for some, and mask underlying causes. Families deserve full, balanced conversations and root-cause strategies—better minerals, protein sufficiency, gut repair, inflammatory trigger identification, and stress modulation—before defaulting to suppression.
